A New Molecular Approach to Prostate Cancer Treatment
The Pochapsky Labratory is examining how enzymes are reshaping cancer research.
Prostate cancer drugs have saved countless lives, but even the best-known treatments come with a long-standing problem: They often affect far more of the body than they should. Medication meant to shut down one enzyme responsible for producing testosterone, the hormone that fuels prostate tumor growth, can end up blocking several other enzymes that have nothing to do with cancer. This broad action leads to serious side effects including liver damage and hormonal imbalance. Inside Prof. Thomas Pochapsky’s (CHEM/BCHEM) Laboratory at Brandeis University, chemical biology major Talia Lazar ’26 has spent more than a year investigating a more precise molecular approach that could eventually help avoid these complications.
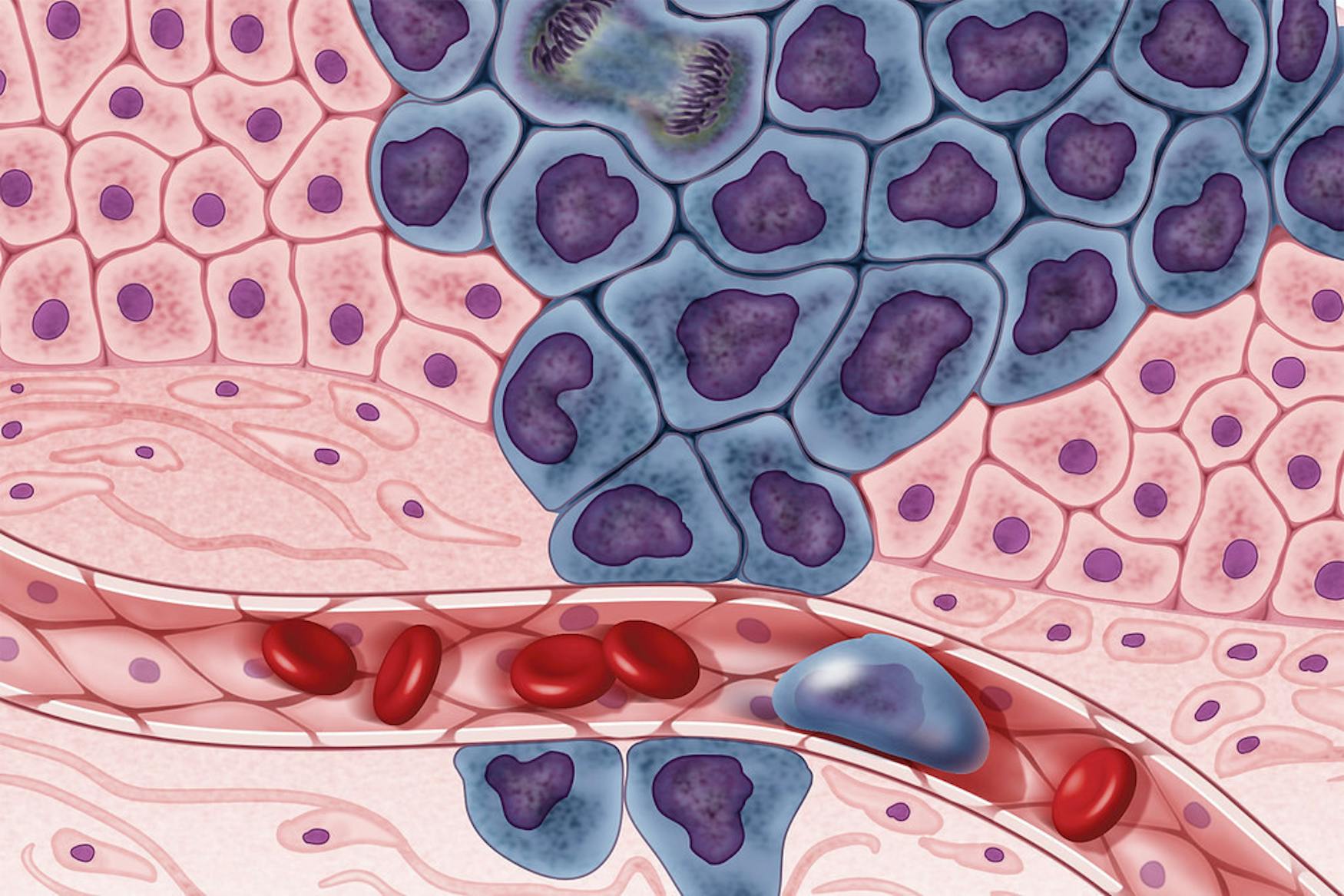
Lazar studies CYP17A1, a member of the cytochrome P450 family of enzymes found in the liver. These enzymes, she explained in an Aug. 25 interview with The Justice, “are vital for hormone balance and drug metabolism.” CYP17A1 plays a central role in making testosterone, so without it, the body cannot produce the hormone. Since testosterone is one of the main drivers of prostate cancer growth, blocking CYP17A1 has become a major strategy in treatment. Drugs like abiraterone do this effectively, but their flexible chemical structures allow them to bind not only to CYP17A1 but to many other enzymes. This broad activity is what causes many of the side effects that patients experience and it is exactly the issue Lazar’s project is working to address.
The Pochapsky Lab studies a different type of molecule called an isonitrile inhibitor. Unlike abiraterone, which can bind where it shouldn’t, isonitriles attach to enzymes only if they match a very strict angle and orientation.
“If it doesn’t bind exactly at 180 degrees, it won’t do it. It will pop off,” Lazar said. This strict requirement makes isonitrile-based molecules far more selective. However, early tests showed that although the compound was more selective, some of its inhibitive abilities might have been compromised. When compared directly to abiraterone, she said, “We found that it’s not as good as an inhibitor.”
Lazar spent last summer working on optimizing the isonitrile’s function, aiming to improve its ability to bind to and inhibit CYP17A1. She and Professor Thomas Pochapsky added a hydroxyl group to the molecule, a small chemical feature that can strengthen binding interactions and serve as a site to attach additional components. “Having that hydroxyl group is a good handle to add other things,” she explained. This change improved how the inhibitor interacted with CYP17A1 and also created opportunities to expand the molecule in new ways.
Those opportunities became important when the team began thinking beyond inhibition altogether. Traditional drugs work only as long as they can block a protein, but cancer cells are adaptable. Over time, they often develop ways to overcome inhibitors: by producing more of the enzyme, changing its structure or switching to alternate pathways. As a result, Lazar and Pochapsky began exploring a newer technology called PROTACs, short for Proteolysis Targeting Chimeras. These molecules aim not just to block harmful proteins but to remove them completely from the cell.
PROTACs have two ends joined by a chemical linker. One end attaches to the target protein, in this case, CYP17A1, while the other end attaches to an E3 ligase, a cellular machine responsible for tagging proteins for destruction. As Lazar explained, when the two are brought together, the ligase “basically tells the cell, okay, you need to chop this up.”
Once E3 tags CYP17A1, the cell uses its proteasome to break down the enzyme entirely. One major advantage of PROTACs is that they can be reused: After a protein is destroyed, the PROTAC can move on to tag another one. “You can reuse the PROTAC again,” Lazar said, “so it recycles and it can attack another enzyme.”
To turn her improved inhibitor into a PROTAC, Lazar needed to physically connect it to the PROTAC’s other half, the part that recruits the E3 ligase. Over the summer she produced a complete PROTAC molecule, which the lab then sent for testing to see whether it could successfully degrade CYP17A1.
But the test results showed a setback. “We tested it in vitro and found no activity with the enzyme,” Lazar said. The issue likely comes down to distance: The site targeted for binding on CYP17A1 sits so deep in the cell’s membrane that the PROTAC couldn’t physically reach it. “We’re thinking that’s because the active site is buried too deep,” she explained, “so the linker is just not long enough to reach.” To solve this, the lab plans to try PROTAC designs with longer linkers and repeat the experiment.
The lab’s size has played a major role in the pace and structure of the work. Beyond Lazar, the lab only has two graduate students, meaning that the lab has to move efficiently and focus only on what shows the most promise.
Although still in its early stages, the project points toward an exciting direction. PROTACs are widely viewed as a potentially transformative tool in cancer therapy, offering a way to eliminate harmful proteins instead of temporarily suppressing them. Applying this technology to CYP17A1 could one day lead to a more selective, longer-lasting prostate cancer treatment with fewer side effects.
For Lazar, the experience of taking on such a large project as the only undergraduate researcher has been meaningful. At the same time, it has left her thinking about the future. While she is interested in drug development, she is not ready to commit to a specific career path. “I think I can take a gap year or two and, like, figure that out,” she said.


Please note All comments are eligible for publication in The Justice.