Implement change in current blood donation policies
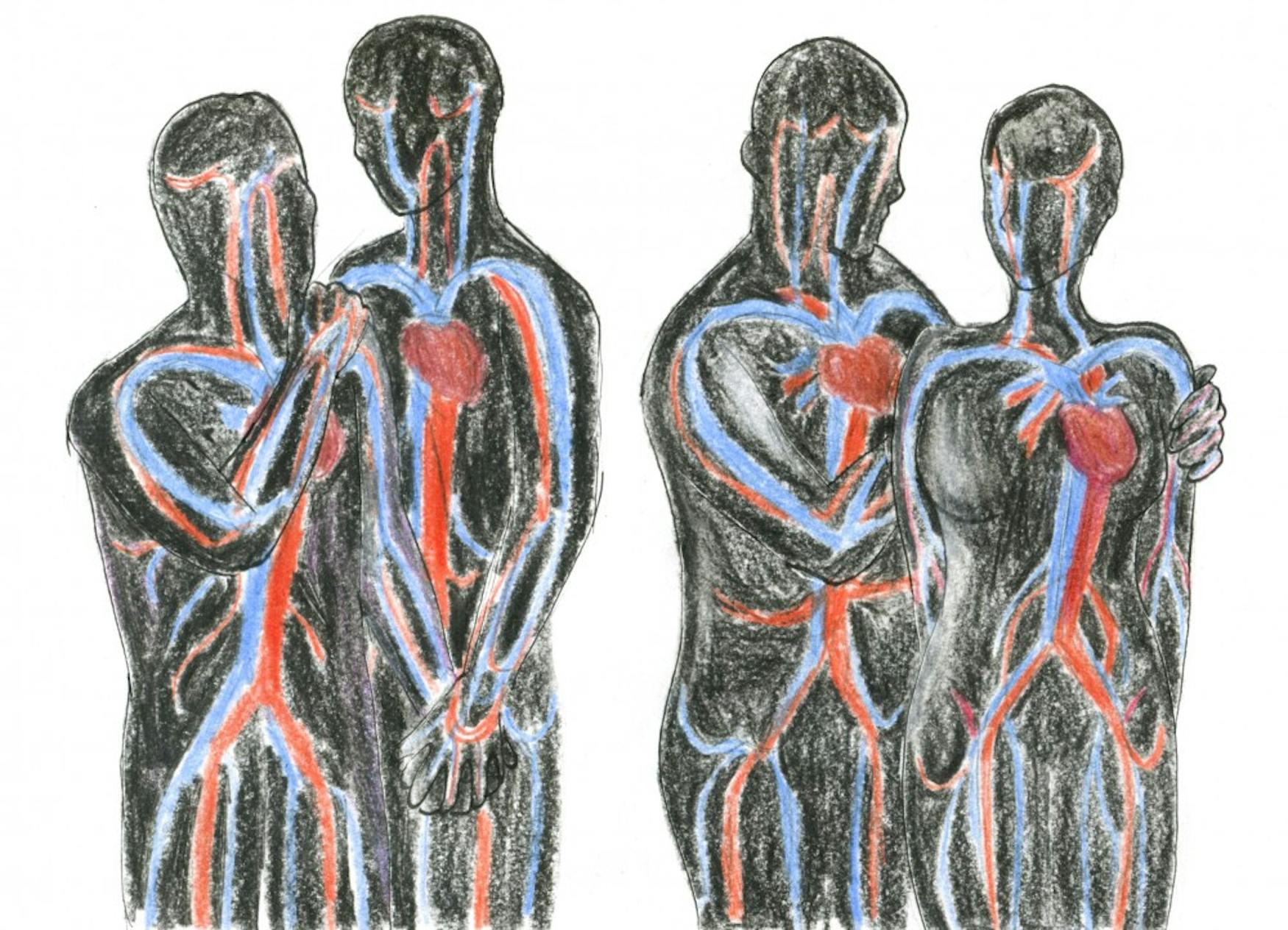
Early in the 1980s, the United States faced an HIV/AIDS epidemic. Not much was known about the emergent virus, except the misconception that it was a “gay plague.” The original disease was called Gay-Related Immune Deficiency, but soon, as cases outside of the gay community started to sprout, the disease was referred to as Acquired Immune Deficiency Syndrome. In 1983, the Food and Drug Administration issued the first blood donor deferral policy, which prohibited men who have sex with men (MSM) from donating blood if they have had a single sexual encounter with another man any time since 1977. According to the American Red Cross, the U.S. is in a constant shortage of blood; with someone requiring a blood transfusion about every two seconds, the ban could pose an obstacle to saving more lives, not to mention that it is inherently prejudiced.
In 2014, the American Red Cross, American Association of Blood Banks and America’s Blood Centers issued a joint statement calling for modification of the lifetime deferral and further consideration of a twelve-month deferral for MSM. The statement claims that “AABB, America’s Blood Centers and the American Red Cross believe the current lifetime deferral for men who have had sex with other men should be modified and that donor deferral criteria should be made comparable with criteria for other behaviors that pose an increased risk for transmission of transfusion-transmitted infections.”
In 2015, the FDA revised the long-lasting policy, placing MSM on a “deferral” period that now prevents male donors from giving blood for 12 months after their last sexual encounter with another man, instead of the permanent ban that was imposed previously, according to a Dec. 21, 2015 press statement. While the policy certainly has allowed more men to donate blood, there are still many more who are not eligible simply because they are sexually active with other men.
Since the Supreme Court’s legalization of same-sex marriage has increased to 61 percent in the U.S., according to a Gallup poll. Two years after the decision, more members of the LGBTQ community, including gay men, are living in monogamous relationships — a ten percent increase in the two years after the decision was made.
When the policy change was announced, Sen. Tammy Baldwin (D-Wis.), the first openly gay senator in the U.S., called the rules “a first step” but lamented that the “revision doesn’t go far enough,” in a Dec. 21, 2015 press release. Baldwin also stated that she will continue to push for the formation of a policy that will be based on individual risk factor and that will not unfairly single out one group of individuals.
Yet as of 2014, the Centers for Disease Control and Prevention — the most up to date collection of data — indicates that gay and bisexual men still account for 82 percent of HIV diagnoses among males aged 13 and older and 67 percent of total new diagnoses in the U.S. The FDA cites the high prevalence of HIV in the MSM population compared to the general population as support for the deferral policy.
It is true that HIV is identified more commonly in MSM than in other demographics; nonetheless, advanced research and modern technology have effectively minimized the risk of transmission. According to an Oct. 26 article in The Baltimore Sun, donated blood is shelved for nine days during the window of infection and “nucleic acid testing can determine with outstanding accuracy whether blood is infected.” In addition, if taken daily, FDA-approved pre-exposure prophylaxis can reduce risk of infection by 90 percent, a value that only increases when combined with condom use. Today, there is plenty of technology available to us, so HIV status is easier to detect. The MSM policy would make sense in the midst of worldwide hysteria, such as the one in the ’80s and the epidemic crisis, but the policy is unfit for our times. Now we know what HIV/AIDS is and have at our disposal a good amount of preventive tools.
At Brandeis, the Waltham Group Blood Drive organizes three blood drives throughout the academic year: one during the the fall semester and two during the spring semester. The group’s main mission is to “collect as many pints of blood as possible as each pint can save up to three lives, or five babies,” according to the group’s website.
When asked about the policy and whether it should be changed, Khushee Nanavati ’19, one of the coordinators of the blood drive, said, “One hundred and ten percent. Everyone on our e-board always talks about it.” Nanavati added that, in the past, the club has tried to protest against the MSM policy: “That’s basically why we had the [‘Love is Love’ themed] drive last time. We were really against it, and we we wanted to spread awareness about this cause.” The theme did not go unnoticed: “We did get in trouble with the Red Cross for having such a controversial theme, so we were red-listed for that,” said Nanavati. Being “red-listed” by the Red Cross, signifies that, from then on, the foundation will “have to approve all of our themes.”
Despite the fact that the American Red Cross signed the joint back in 2014 to fight the previous policy from 1977, they seem to be fine with the twelve-month deferral, or at least at the moment, they are not doing anything about it. Perhaps the Red Cross might be against the twelve-month policy, but they are still adhering to the current policy. There is no fight back on their part. Furthermore, the club did not feel impeded to try and come up with other alternatives in order to not depend so much on the American Red Cross to host the blood drives. They have sought to partner up with other humanitarian organizations, but the search thus far has been futile.
“We did want to change it, but we weren’t able to find anyone who gave us the benefits that Red Cross did and did it for free. We otherwise would have to pay for it. Red Cross gives us posters, nurses, food, data, every single thing. The other organizations aren’t as big and as powerful to do that,” Nanavati said.
According to a study conducted by the Williams Institute — “UPDATE: Effects of Lifting Blood Donation Bans on Men who Have Sex with Men” by Ayako Miyashita and Gary J. Gates — lifting the ban would have a positive outcome by increasing the total of annual blood supply from 2 to 4 percent. The study also reveals that “if the current MSM ban were completely lifted an estimate of additional 360,000 men would likely donate 615,000 additional pints of blood each year.”
In the wake of an emergency like the Las Vegas massacre or a natural disaster such as Hurricane Harvey, blood donation is critical, according to the American Red Cross. The quotidian reality is that times are always uncertain, but at least in today’s times, we possess information that we did not have a few decades ago. As a result, it is the right time for the MSM policy to remain as part of the past, since it can only be the residue of an ignorant and prejudiced decade, and its prevalence is preventing lives from being fully lived.



Please note All comments are eligible for publication in The Justice.